Stroke is the nation's fifth-leading cause of death, and is a leading cause of adult disability. When the brain is under attack by a stroke, getting the right treatment as quickly as possible is critical. As part of the first Joint Commission-accredited Comprehensive Stroke Center in the state, the team at Memorial Hermann-Texas Medical Center's Mischer Neuroscience Institute is specially trained to do just that.
The Stroke Center's Scope of Expertise
- Cerebral thrombosis
- Cerebral embolism
- Intracerebral hemorrhage
- Subarachnoid hemorrhage
- Cerebrovascular surgery
- Transient ischemic attack
- Carotid and vertebral artery stenosis
- Cardiac causes of stroke
- Genetically-based stroke disease
- Immunological causes of stroke
- Coagulation (blood clotting) disorders
- Stroke in young patients
- Vascular dementia
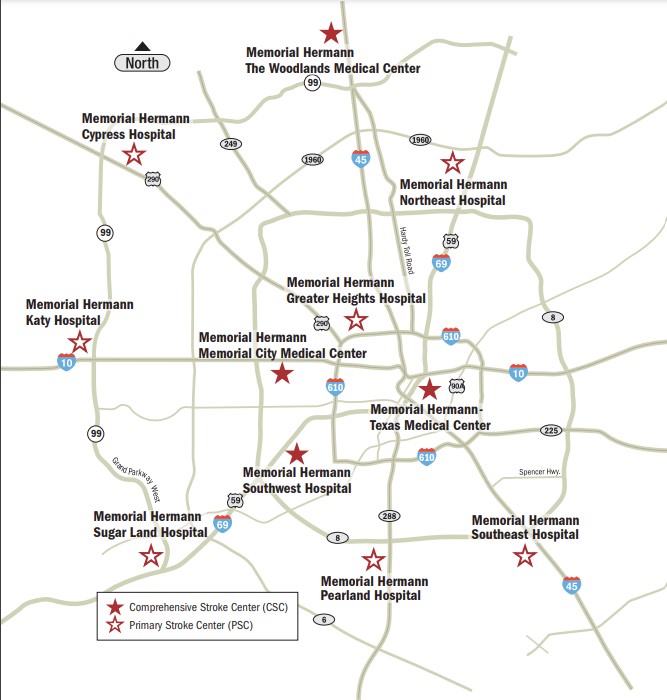
First Network of Accredited Stroke Centers
We were the first network of accredited Stroke Centers in the region and among fewer than 30 in Texas. Our network of Memorial Hermann Stroke Centers also enables Memorial Hermann ER's to receive stroke patients transferred via ground or Life Flight air ambulance from hospitals lacking the capability or capacity to provide urgent treatment.
Memorial Hermann-TMC is also the region's leading on-site, 24/7 dedicated stroke team offering patients comprehensive treatment around the clock.
Locations with Comprehensive Stroke Certification
Types of Stroke
There are two major types of stroke: ischemic stroke and hemorrhagic stroke.
Ischemic Stroke
An ischemic stroke occurs when an artery is blocked by a blood clot. This type of stroke may result from clogged arteries, called atherosclerosis. When fat, cholesterol and other substances collect on the artery walls, they form a sticky substance called plaque, which over time builds up and makes it hard for blood to flow properly to the brain.
Hemorrhagic
A hemorrhagic stroke occurs when a blood vessel in part of the brain becomes weak and bursts open (a brain aneurysm), causing blood to leak into the brain.
Stroke: What You Need to Know
NIH Grants
As pioneers in treating acute stroke, our team members are the recipients of more than $2 million annually in National Institutes of Health (NIH) grants for stroke research. We were the first in Houston and one of the first in the country to use the clot-dissolving drug Alteplase for acute strokes. When given Alteplase within three hours of the onset of stroke symptoms, patients are at least 33% more likely to recover from a stroke with little or no disability.
Stroke Symptoms
Symptoms of a stroke vary depending on the type of stroke and what part of the brain is damaged. Common symptoms of a stroke include:
- Blurred vision, brief blindness, or double vision
- Severe headache (typically seen with hemorrhagic stroke)
- Difficulty speaking
- Confusion or loss of memory
- Difficulty writing or reading
- Temporary memory problems
- Muscle weakness on one side of your body
- Vertigo (like the room is spinning) and dizziness
- Trouble speaking or understanding others who are speaking
- Strange sensations, such as burning or tingling
- Trouble with coordination, clumsiness
- Loss of consciousness
- New or changed headache
B.E. F.A.S.T.
Call 911 if you or someone you know has symptoms of stroke. Brain function can be saved if you are having a stroke and get help quickly. The acronym B.E. F.A.S.T. can be helpful in remembering the warning signs and taking the appropriate action.
- BALANCE: Is there a sudden loss of balance or coordination?
- EYES: Is there sudden double or blurred vision and/or sudden trouble seeing that persists?
- FACE: Ask the person to smile. Is one or both sides drooping?
- ARMS: Ask the person to raise both arms. Does one side drift downward? Weakness or numbness on one side?
- SPEECH: Does the person have slurred/garbled speech? Can he/she repeat simple phrase?
- TIME: If you observe any of these signs, call 911 immediately and note time symptoms began.
Risk Factors for Stroke
In many cases, a stroke can be prevented. Certain diseases or conditions increase your risk of stroke. Some risk factors for stroke include those you can and cannot change.
These factors include:
- Atrial fibrillation (an abnormal heart rhythm)
- Diabetes. Patients with diabetes are at an increased risk for stroke compared to people without diabetes. The circulation problems associated with this disease may be responsible for poorer outcomes in people with diabetes following stroke.
- Family history of stroke
- Heart disease
- High blood pressure. High blood pressure is the number one risk for strokes.
- High cholesterol. High cholesterol can lead to hardening of your arteries (atherosclerosis), which can result in clogged arteries.
- Smoking. Smoking increases the risk of most types of strokes.
- Obesity
- Diet. People who eat more fruits, vegetables, fish and whole grains may have a lower risk of stroke that people who eat lots of refined grains, red meat and increased sodium levels.
- Illegal drug use, such as cocaine
- The use of some medications, such as birth control pills, can increase the chance of blood clots in women.
Become familiar with your stroke risk factors and learn the symptoms of a stroke. BE FAST – this step can mean the difference between life and death for you or a loved one.
Stroke in Women
Stroke has affected approximately 4 million females in the United States, yet a recent survey reveals that one in five American women can’t identify the warning signs.
Stroke Risk Factors for Women
Several special factors put women at risk for stroke. A 10-fold increase in stroke risk is associated with women who experience migraines with aura. Pre-eclampsia, a blood-pressure disorder that sometimes occurs during pregnancy, also doubles a woman’s stroke risk. Even if successfully treated for preeclampsia or high blood pressure while pregnant, women who have had this condition should be monitored for the rest of their lives.
Similarly, women 75 and older should be regularly examined for atrial fibrillation (irregular heartbeat) as females with this condition are four to five times more likely to experience a stroke.
Risk factors for stroke common to both males and females include obesity, tobacco use, and high blood pressure.
Imaging Studies and Other Tests for Stroke
While physical examination helps physicians determine the type of stroke suffered by a patient, other tests can provide more detailed information regarding treatment. Our stroke team can precisely identify, localize and determine the cause of strokes and other brain lesions using advanced MRI and CT techniques, and can then determine whether treatment will benefit or harm the individual patient.
We are also world leaders in the use of ultrasound both to diagnose and help dissolve the blood clots that cause most strokes.
Some common tests include:
Computed Tomography (CAT Scan) A CAT, or CT, scan uses a computer system to give a detailed picture of brain tissue. This test can determine whether a stroke was caused by bleeding in the brain or a blood vessel blockage. When available, a CT scan typically is one of the first tests performed on stroke patients. During the test, the patient lies on a table with his or her head in a large, donut-shaped machine that takes pictures of the brain. A CT scan generally takes approximately 15 minutes to complete and is painless.
Magnetic Resonance Imaging (MRI) An MRI uses a large magnetic field and radio waves to give physicians a 3-D picture of the brain. During an MRI, which is painless, a patient must lie still within the MRI scanner for approximately 30 minutes. Because the MRI provides such a sharp image of the brain, it is especially useful in identifying smaller strokes.
Ultrasound of the Carotid Arteries (Doppler) A Doppler ultrasound allows physicians to view the primary neck arteries and any blockages or narrowing due to atherosclerosis. During the test, a technician slowly moves a probe around the outer surface of a patient’s neck. This probe gathers detailed information and sends it to a computer for analysis. This ultrasound takes approximately 45 minutes to complete and is painless.
Lumbar Puncture A physician performs a lumbar puncture, or spinal tap, to obtain a sample of the normally clear fluid that circulates around the brain and spinal cord. A doctor generally does this procedure at the bedside with the patient lying on his or her side. The health care team will inject local anesthetics in the lower back and then insert a thin needle to gather cerebrospinal fluid. As headaches may arise following the test, patients are encouraged to drink plenty of fluids and ask their nurse for pain medication, if needed.
Echocardiogram During an echocardiogram, a technician slowly moves a probe over the surface of the chest to gather pictures of the heart. This procedure helps the health care team evaluate the size of a patient’s heart, the condition of the heart valves and the motion of the heart wall. The test takes approximately one hour to complete and is painless.
Transesophageal Echocardiogram (TEE) ATEE provides physicians with an even more accurate view of a patient’s heart. To perform the test, the health care team provides medication to relax the patient and numb his or her throat, then asks the patient to swallow a probe. This test can gauge the severity of certain valve problems and help detect infection of the heart valves, certain congenital heart diseases – such as a hole between the upper chambers of the heart, known as atrial septal defect – and a tear or dissection of the aorta.
Electrocardiogram (EKG) An EKG produces an image of the heart’s electrical activity. To perform the test, a technician places wires on the surface of a patient’s chest and limbs. This test takes approximately 10 to 15 minutes and is painless.
Electroencephalogram (EEG) An EEG is a painless test that takes approximately 45 minutes to complete and records the electrical activity of the brain. The health care team will measure a patient’s head and place electrodes on the scalp in preparation for the test. During the test, the patient will be asked to take several deep breaths and may be shown a strobe light that flashes at different speeds. Physicians also may want to observe brain patterns that occur during sleep. An EEG helps physicians diagnose a variety of neurological problems, including common headaches, dizziness, seizure disorders, strokes and degenerative brain disease.
Cerebral Angiography or Arteriography During this procedure, the health care team injects special dyes into the blood vessels of the head and neck. The dye in the blood vessels shows up on X-rays and indicates the size and location of any blockages. A physician generally will perform this test only if a patient is having surgery such as a carotid endarterectomy to remove the blockage, or if other tests have not provided sufficient information.
Neuro Critical Care and Stroke Units
Neurointensivists and experienced mid-level practitioners staff our dedicated 32-bed Neuro Critical Care Unit and 12-bed Stroke Unit, around the clock to provide ongoing intensive care to critically ill patients. We manage more neurotrauma cases than any other center in the southwestern United States, and we are internationally recognized for the treatment of high-acuity brain and spinal cord injuries.
Thrombolytic Quality Record
Working closely with the Houston Fire Department and local EMS services, the Stroke Center’s team has an impressive track record of success in the administration of thrombolytic therapy.
25% of patients who present with ischemic stroke receive thrombolytic therapy; that is more than 10 times the national average of 2 to 3%. Because 80% of strokes are caused by cerebral thrombosis, the thrombolytic advantage is an important one.
Endovascular Therapy
Using advanced MRI and CT imaging, the Stroke Center's team has the capability to thread tiny catheters into the arteries of the brain to extract the clots causing strokes. This approach allows for reversal of damage in patients who arrive too late for intravenous Tenecteplase but within eight hours of symptom onset.
Contact Us
Please fill out the fields below, and we will contact you.